Non Alcoholic Fatty Liver Disease Solution NAFLD treatment plan
Introduction
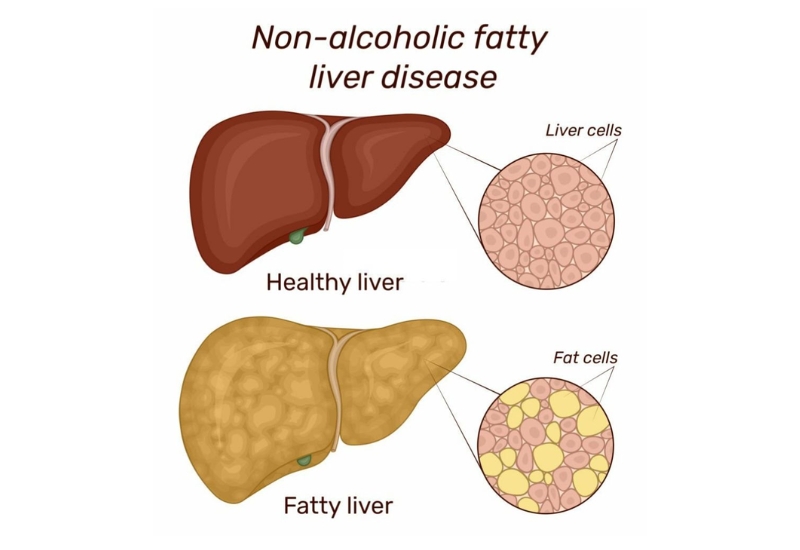
Non-alcoholic fatty liver disease (NAFLD) refers to the accumulation of fat in the liver without significant alcohol consumption. This condition is becoming increasingly common worldwide, largely due to rising rates of obesity, diabetes, and unhealthy diets. NAFLD ranges from simple fatty liver, which is often harmless, to more severe forms like non-alcoholic steatohepatitis (NASH), which can lead to liver damage, cirrhosis, and even liver failure.
NAFLD is generally asymptomatic, which means that individuals may not realize they have the condition until it progresses. Early detection and intervention are crucial in managing the disease and preventing more severe liver damage.
In this article, we will explore a comprehensive NAFLD treatment plan that can help manage and even reverse the condition. This treatment plan includes lifestyle changes, dietary recommendations, exercise, medical treatments, and additional holistic approaches based on the principles outlined in Julissa Clay’s Non-Alcoholic Fatty Liver Disease Solution.
Understanding the Causes and Risks of NAFLD
To understand how to treat NAFLD effectively, it is essential to first understand the underlying causes and risk factors. NAFLD primarily results from an imbalance between fat storage and fat burning in the liver.
Risk Factors of NAFLD
- Obesity: Excess fat, especially abdominal fat, is a leading contributor to fat accumulation in the liver. Obesity is the most significant risk factor for the development of NAFLD.
- Insulin Resistance and Type 2 Diabetes: Individuals with insulin resistance or type 2 diabetes are at higher risk of developing NAFLD, as insulin resistance promotes fat storage in the liver.
- High Blood Sugar and High Cholesterol: Elevated triglycerides, high cholesterol levels, and abnormal lipid profiles can contribute to fat buildup in the liver.
- Metabolic Syndrome: This refers to a group of conditions including high blood pressure, excess abdominal fat, high blood sugar, and abnormal cholesterol levels. Individuals with metabolic syndrome are at a higher risk of developing NAFLD.
- Poor Diet: Diets rich in processed foods, sugars, and unhealthy fats can promote fat accumulation in the liver.
- Genetics: Family history and genetic predisposition can also play a role in the development of NAFLD.
- Age and Gender: NAFLD is more common in middle-aged individuals, and while it can affect both men and women, men tend to develop more severe forms of the disease.
Progression of NAFLD
NAFLD can progress through several stages:
- Simple Fatty Liver (NAFL): This is the early stage of NAFLD where there is an accumulation of fat in the liver cells but no inflammation or damage. Simple fatty liver generally does not cause liver dysfunction and may not lead to serious complications.
- Non-Alcoholic Steatohepatitis (NASH): In this stage, fat accumulation is accompanied by inflammation and liver cell damage. NASH can lead to fibrosis (scarring of the liver) and, if left untreated, may progress to cirrhosis.
- Cirrhosis: In the final stage of NAFLD progression, the liver becomes severely scarred and loses its ability to function properly. Cirrhosis can lead to liver failure, requiring a liver transplant.
Understanding the stages of NAFLD helps emphasize the importance of early intervention through lifestyle changes, diet, and treatment.
Lifestyle Changes for Managing NAFLD
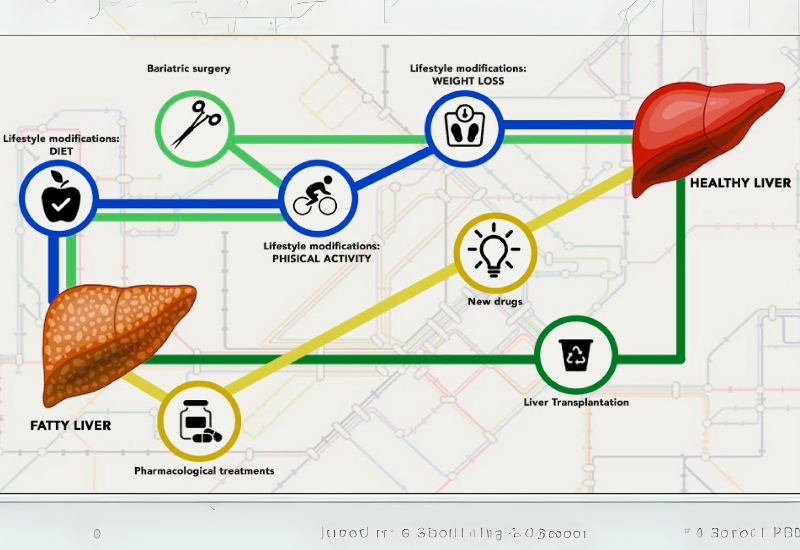
One of the most effective ways to manage NAFLD is by implementing significant lifestyle changes. These changes can help reduce liver fat, improve liver function, and prevent progression to more severe stages.
Weight Loss and Obesity Management
Losing weight is one of the most beneficial steps for those with NAFLD, particularly if obesity is a contributing factor. Reducing body fat, especially abdominal fat, can improve insulin sensitivity, reduce liver fat, and lower inflammation.
Julissa Clay’s Approach to Weight Loss: Julissa Clay’s Non-Alcoholic Fatty Liver Disease Solution emphasizes a gradual and sustainable weight loss of 5-10% of total body weight. Research shows that this level of weight loss can significantly improve liver health and reduce the risk of progression from NAFLD to NASH.
Exercise and Physical Activity
Regular exercise is vital for managing NAFLD. Physical activity helps to reduce body fat, increase muscle mass, improve insulin sensitivity, and promote overall liver health. Both aerobic exercises (e.g., walking, cycling, swimming) and resistance training (e.g., weightlifting) are beneficial.
Exercise Recommendations for NAFLD:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
- Incorporate strength training exercises at least two days a week.
- Include flexibility exercises such as yoga or stretching to improve muscle balance.
Exercise not only helps in fat loss but also has anti-inflammatory effects, which can help reduce liver inflammation.
Stress Reduction
Chronic stress can exacerbate insulin resistance and contribute to fat buildup in the liver. Therefore, managing stress is an important aspect of managing NAFLD.
Stress-Reduction Techniques:
- Mindfulness Meditation: Practice mindfulness meditation to calm the mind and reduce stress. Meditation can help lower cortisol levels, improve sleep, and reduce inflammation.
- Deep Breathing Exercises: Deep breathing techniques can help activate the parasympathetic nervous system, leading to relaxation and stress relief.
- Yoga and Tai Chi: These practices combine movement, breathing, and meditation, all of which help reduce stress levels and improve overall well-being.
Nutritional Plan for NAFLD Treatment
Diet plays a critical role in managing NAFLD. A nutrient-rich, balanced diet can reduce liver fat, inflammation, and promote weight loss.
Dietary Recommendations for NAFLD
A liver-friendly diet should focus on whole foods, healthy fats, lean proteins, and high-fiber carbohydrates. It’s also crucial to reduce intake of refined sugars, unhealthy fats, and processed foods.
Foods to Include:
- Leafy Greens and Vegetables: Vegetables like spinach, kale, broccoli, and Brussels sprouts are rich in antioxidants and fiber, which can support liver detoxification and reduce inflammation.
- Healthy Fats: Incorporate healthy fats such as those found in olive oil, avocados, nuts, and seeds. Omega-3 fatty acids, found in fatty fish (salmon, sardines, mackerel), flaxseeds, and chia seeds, can help reduce liver fat.
- Whole Grains: Whole grains such as quinoa, brown rice, and oats are high in fiber and help to regulate blood sugar levels.
- Lean Protein: Sources of lean protein like poultry, fish, legumes, and tofu can help build muscle mass without burdening the liver with excess fat.
- Low Glycemic Index Foods: Foods with a low glycemic index, such as sweet potatoes, beans, and most vegetables, help regulate blood sugar levels, which is important for managing insulin resistance and preventing NAFLD progression.
Foods to Avoid:
- Refined Carbohydrates and Sugars: Minimize intake of sugary foods and drinks (e.g., soda, sweets, pastries) and refined grains (e.g., white bread, pasta) as they can lead to weight gain, insulin resistance, and liver fat accumulation.
- Trans Fats: Avoid trans fats found in processed foods, fried foods, and many packaged snacks. These fats are harmful to both the liver and cardiovascular health.
- Alcohol: Even though NAFLD is not caused by alcohol consumption, it is essential to limit alcohol intake, as it can worsen liver inflammation and damage.
The Mediterranean Diet: A Recommended Approach
Many experts recommend the Mediterranean diet for individuals with NAFLD. This diet emphasizes fresh vegetables, fruits, whole grains, legumes, nuts, seeds, and healthy fats such as olive oil. The Mediterranean diet is rich in antioxidants, fiber, and healthy fats, making it ideal for liver health.
Incorporating anti-inflammatory foods, such as garlic, turmeric, ginger, and green tea, can also be beneficial. These foods may help reduce liver inflammation and promote detoxification.
Medical Interventions for NAFLD
While lifestyle changes and diet are the primary approaches to managing NAFLD, there may be cases where medical treatment is necessary.
Medications for NAFLD
Currently, there are no FDA-approved medications specifically for NAFLD, but some medications are prescribed off-label to help manage the condition:
- Insulin Sensitizers: Medications such as metformin or thiazolidinediones (TZDs) may be used to improve insulin sensitivity in individuals with diabetes or insulin resistance.
- Vitamin E: In some cases, high doses of vitamin E have been shown to reduce liver inflammation in people with NASH.
- Statins: For individuals with high cholesterol or cardiovascular risk, statins may be prescribed to help manage lipid levels and prevent further liver damage.
However, medications are typically used when lifestyle changes alone are insufficient or when the disease has progressed to more severe stages like NASH or cirrhosis.
Monitoring and Liver Function Tests
For individuals diagnosed with NAFLD, regular monitoring of liver function through blood tests is essential. This includes measuring liver enzymes (ALT, AST), bilirubin, and other markers that assess liver health.
Imaging techniques such as ultrasound, CT scans, or MRI can also be used to assess liver fat content and detect signs of fibrosis or cirrhosis.
Conclusion
Non-Alcoholic Fatty Liver Disease (NAFLD) is a serious yet manageable condition that requires a holistic approach to treatment. Lifestyle changes such as weight loss, exercise, and stress management are foundational to managing the disease. A nutritious, liver-friendly diet that includes anti-inflammatory foods is also crucial.
Medical treatments and regular monitoring are important for individuals with more advanced stages of NAFLD. Combining these treatments with alternative therapies, such as herbal supplements and acupuncture, can offer additional benefits.
By following a comprehensive treatment plan based on lifestyle adjustments, nutrition, medical interventions, and holistic therapies, individuals with NAFLD can significantly improve their liver health, prevent disease progression, and enhance overall quality of life.











