Top ways The Shingles Solution reduces nerve pain.
What is Shingles?
Shingles, also known as herpes zoster, is a viral infection that manifests as a painful rash, often in a stripe-like formation on one side of the body. Caused by the varicella-zoster virus—the same virus responsible for chickenpox—shingles can emerge years or even decades after the initial infection. Once someone has had chickenpox, the varicella-zoster virus lies dormant in the nervous system. Later in life, it may reactivate, resulting in shingles. Though not life-threatening, shingles can cause significant pain, and the risk of complications increases with age.
This guide delves into the causes, symptoms, risk factors, and treatment options for shingles, offering a comprehensive look at ways to manage this condition and minimize its impact on daily life.
Symptoms of Shingles: Identifying the Signs
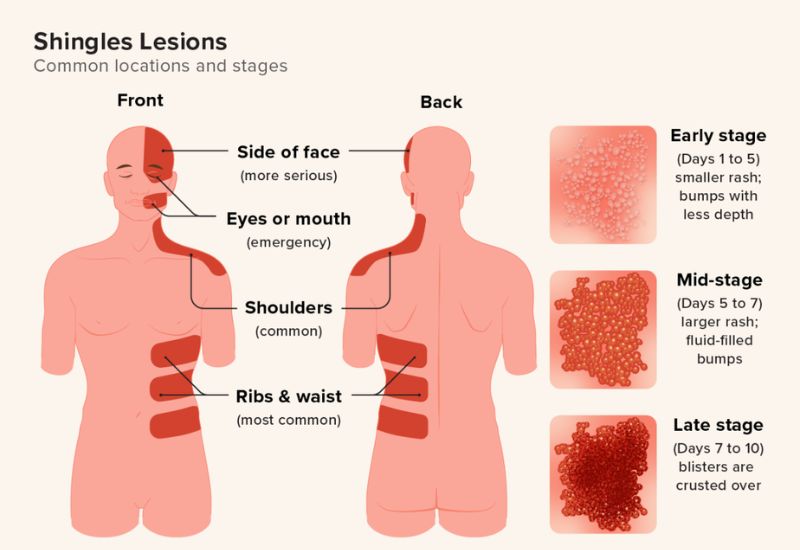
Shingles symptoms typically affect only a small section on one side of the body. Here’s an overview of the most common signs:
- Pain and Tingling: Pain is often the first symptom, described as burning, tingling, or itching in a localized area.
- Sensitivity to Touch: The affected skin area may become highly sensitive, with even light touch causing discomfort.
- Red Rash: A few days after the initial pain, a rash appears. The rash forms as red blotches and then progresses to fluid-filled blisters.
- Blisters and Crusting: The blisters eventually burst, crust over, and heal within two to four weeks, although pain may persist.
- Additional Symptoms: Fever, headache, fatigue, and sensitivity to light may accompany the rash.
Location of Shingles Rash: Shingles commonly appears as a stripe of blisters wrapping around the torso, but it may also occur on the face, around one eye, or on one side of the neck.
Understanding Nerve Pain in Shingles
To fully appreciate how The Shingles Solution works, it’s important to first understand the nature of nerve pain in shingles and postherpetic neuralgia (PHN).
1 The Role of the Varicella-Zoster Virus
After an initial chickenpox infection, the varicella-zoster virus (VZV) remains dormant in the body’s nerve tissues, typically in the spinal cord or brainstem. Years later, the virus can reactivate, often triggered by factors such as stress, weakened immunity, aging, or other health conditions. When the virus reactivates, it travels along nerve fibers to the skin, causing the characteristic rash and painful blisters of shingles.
The nerve pain in shingles is caused by the inflammation and damage the virus inflicts on the nerve cells. The infection affects the sensory nerves, which are responsible for transmitting sensations such as touch, temperature, and pain to the brain. As the virus damages these nerves, it can lead to abnormal nerve signaling, resulting in pain that may persist long after the rash has healed.
2 Postherpetic Neuralgia (PHN)
In some cases, the pain from shingles persists even after the rash has resolved. This condition, known as postherpetic neuralgia (PHN), is characterized by lingering nerve pain that can last for months or years. PHN is one of the most debilitating aspects of shingles, as it significantly affects a person’s quality of life, causing chronic pain, sleep disturbances, and difficulty with daily activities.
The pain associated with PHN can be difficult to treat. It may manifest as a burning, stabbing, or aching sensation, and can even be triggered by light touch or temperature changes. In severe cases, individuals may develop allodynia, a condition where even non-painful stimuli, such as a breeze or a soft touch, cause intense pain.

How The Shingles Solution Works
The Shingles Solution is not a single treatment, but rather a comprehensive approach to managing nerve pain associated with shingles. It often includes a combination of medical treatments, natural remedies, physical therapies, and lifestyle modifications that work together to reduce inflammation, promote healing, and manage pain. The following are the top ways The Shingles Solution reduces nerve pain in shingles:
1 Antiviral Medications
Although antiviral medications do not directly relieve nerve pain, they play an essential role in controlling the shingles infection and preventing its spread. By targeting the varicella-zoster virus, antiviral medications such as acyclovir, valacyclovir, and famciclovir can help reduce the severity and duration of the shingles outbreak. Early treatment with antiviral drugs can also lower the risk of developing postherpetic neuralgia.
By addressing the viral cause of the infection, antiviral medications help to reduce the initial inflammation in the affected nerves. This can, in turn, minimize the extent of nerve damage and lower the likelihood of PHN developing.
2. Pain-Relieving Medications
One of the primary components of The Shingles Solution is pain management. Since shingles and PHN can cause severe nerve pain, a variety of pain-relieving medications are often employed to help individuals cope with the discomfort. Common medications include:
- Anticonvulsants (Gabapentin, Pregabalin): These medications are often prescribed to reduce nerve pain by stabilizing the electrical activity of the nerves. They are particularly effective in treating PHN, as they target the abnormal nerve signals that cause pain.
- Topical Analgesics (Capsaicin Cream, Lidocaine Patches): These topical treatments are applied directly to the affected area of the skin. Capsaicin, derived from chili peppers, works by depleting substance P, a neurotransmitter involved in pain transmission. Lidocaine patches numb the area and block pain signals from the affected nerves.
- Opioid Painkillers (in severe cases): For individuals with severe nerve pain, short-term use of opioid painkillers may be considered. However, due to the risk of dependency and side effects, opioids are typically only used when other treatments have failed.
- Over-the-counter analgesics (NSAIDs, Acetaminophen): For milder cases of pain, nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be effective for reducing inflammation and providing pain relief.
While pain-relieving medications help manage symptoms, they do not address the underlying nerve damage. Therefore, The Shingles Solution also incorporates strategies to heal the nerves and improve long-term outcomes.
3 Nerve Block and Injections
In cases where pain is particularly severe and resistant to oral medications, nerve block injections may be used to provide relief. These injections typically involve the administration of local anesthetics or corticosteroids directly to the affected nerves. The goal is to block pain signals and reduce inflammation in the affected area.
Epidural Steroid Injections may also be considered for patients with severe, localized pain. These injections deliver a potent anti-inflammatory medication directly to the epidural space near the spinal cord, where the affected nerve roots reside. The Shingles Solution may incorporate these injections as a short-term measure to help reduce nerve pain while other treatments work to promote healing.
4 Natural Remedies and Supplements
In addition to conventional medical treatments, The Shingles Solution often includes natural remedies and supplements designed to support nerve healing and reduce inflammation. These remedies are rooted in traditional medicine and have gained popularity due to their non-invasive nature and potential for providing long-term relief.
Some of the most commonly used natural remedies for nerve pain associated with shingles include:
- Capsaicin: Topical capsaicin, as mentioned earlier, is an effective natural remedy for reducing nerve pain. It works by depleting substance P, a neurotransmitter involved in pain transmission. Capsaicin cream or patches can be applied to the affected area to help relieve pain.
- L-Arginine: This amino acid is known for its ability to improve blood circulation. Enhanced blood flow to the affected nerves can promote healing and reduce pain. L-arginine supplements may be used to support the healing of damaged nerves.
- Alpha-Lipoic Acid (ALA): A powerful antioxidant, ALA is thought to protect nerves from oxidative stress and promote nerve regeneration. It may help reduce the severity of pain and improve nerve function in people with postherpetic neuralgia.
- B Vitamins (B1, B6, B12): B vitamins, particularly B12, are critical for nerve health and regeneration. Deficiencies in these vitamins are often linked to nerve damage and pain. Supplementation with B vitamins can support nerve healing and reduce the intensity of nerve pain.
- Turmeric (Curcumin): Curcumin, the active compound in turmeric, has potent anti-inflammatory and antioxidant properties. It may help reduce the inflammation caused by the shingles virus and promote healing of the affected nerves.
These natural remedies can be used in combination with conventional treatments to provide a more holistic approach to managing nerve pain and promoting nerve healing.
5 Stress Reduction and Emotional Support
Chronic pain from shingles and PHN can have a significant emotional and psychological impact on patients. The Shingles Solution often includes stress-reduction techniques and emotional support strategies, as stress and anxiety can exacerbate nerve pain. Some methods to manage stress and improve mental health include:
- Cognitive Behavioral Therapy (CBT): CBT is a type of psychotherapy that helps individuals manage pain and stress by changing negative thought patterns and behaviors. It can be particularly useful for individuals with chronic pain, helping them develop coping strategies and improve their quality of life.
- Mindfulness and Meditation: Mindfulness practices, such as deep breathing exercises and meditation, can help individuals relax and reduce the psychological impact of pain. These techniques can lower cortisol levels, reduce stress, and alleviate the perception of pain.
- Physical Therapy and Exercise: Gentle physical therapy and low-impact exercises can help individuals maintain mobility and reduce muscle tension associated with nerve pain. Physical activity also promotes the release of endorphins, the body’s natural painkillers.
6 Sleep Improvement Strategies
Pain from shingles and PHN often worsens at night, leading to poor sleep quality and exacerbating fatigue and discomfort. Sleep is crucial for the body’s healing process, and improving sleep hygiene is an important part of The Shingles Solution. Strategies for better sleep include:
- Creating a Comfortable Sleep Environment: Ensuring a cool, quiet, and dark environment for sleep can help improve restfulness and reduce the perception of pain at night.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): CBT-I is a specialized form of therapy designed to address sleep disturbances. It can help individuals with chronic pain improve their sleep patterns and enhance their overall well-being.
Prevention: Vaccines and Immunization
Vaccination is the most effective way to prevent shingles or reduce the severity of symptoms if it does occur. Here’s a look at the available options:
- Shingrix: Approved in 2017, Shingrix is recommended for adults 50 and older, even those who have previously received the older Zostavax vaccine or don’t remember having chickenpox. Shingrix is given in two doses, spaced two to six months apart, and has shown over 90% efficacy in preventing shingles and PHN.
- Who Should Avoid the Vaccine?: The shingles vaccine is generally safe but may not be suitable for individuals with certain health conditions, such as those with severe allergic reactions to vaccine ingredients or those currently undergoing stem cell transplants.

Caring for Shingles at Home
Managing shingles symptoms at home involves supportive care to alleviate discomfort and prevent secondary infections:
- Keep the Rash Clean and Dry: Avoid scratching the rash, and cover it loosely to protect the skin.
- Apply Cool Compresses: Cold, moist compresses on the affected area can help soothe burning or itching sensations.
- Take Baths with Oatmeal: Oatmeal baths are known to relieve itching and irritation.
- Wear Comfortable Clothing: Soft, loose clothing can reduce skin irritation.
Contagion and Isolation: Is Shingles Contagious?
Although shingles itself is not contagious, the varicella-zoster virus can spread to someone who has never had chickenpox, causing them to develop chickenpox rather than shingles. Precautions include:
- Avoid Contact with Vulnerable Individuals: People with shingles should stay away from pregnant women, infants, and individuals with weakened immune systems.
- Cover the Rash: Keeping the rash covered reduces the risk of virus transmission.
- Practice Good Hygiene: Regular handwashing helps prevent the spread of the virus.
The Course of a Shingles Outbreak: What to Expect
A shingles outbreak usually follows a predictable pattern from onset to recovery:
- Prodromal Stage: Pain, tingling, or burning sensations begin in a localized area a few days before the rash appears.
- Active Rash Stage: Blisters develop in a band-like pattern, fill with fluid, and then crust over within 7 to 10 days.
- Healing Stage: The scabs fall off, and the skin heals over the following weeks. For some, residual pain (PHN) may persist.
The entire course of a shingles outbreak typically lasts three to five weeks, though complications like PHN can prolong discomfort.
Conclusion: Taking Control of Shingles
Shingles is a painful, sometimes debilitating condition, but with proper management and timely vaccination, its impact can be minimized. For those over 50 or with compromised immunity, vaccination offers significant protection. Early treatment, supportive care, and a strong understanding of shingles can empower individuals to manage symptoms effectively and reduce the risk of long-term complications.

Whether you are managing a shingles outbreak or seeking preventive care, proactive measures can make a difference. By consulting with healthcare providers, understanding the signs and symptoms, and adopting preventive strategies, those at risk of shingles can maintain better control over their











